The Calgary Health Region will post a sizable deficit this year as staffing shortages leave the medical authority with a massive bill for nearly one million hours in overtime, says the region's chief executive.
Despite earlier predictions of a balanced budget, Jack Davis, CEO of the Calgary Health Region, said the CHR will sink into the red in the '07-'08 fiscal year, due to a larger-than-expected pay hike for nurses and $63 million in overtime costs.
Davis would not reveal the anticipated size of the deficit facing the CHR, the body in charge of Calgary's health system including four hospitals. He said it will be larger than last year's $70-million shortfall, which required a government bailout.
"There's no question we'll have a deficit," Davis said in a year-end interview with the Herald.
"It's definitely going to be harder than last year."
The health authority has faced persistent problems finding enough nursing staff in recent years, which has forced local hospitals to close beds and cancel procedures.
Earlier this month, the Alberta Children's Hospital had to reschedule six surgeries in two weeks because there were not enough critical care nurses.
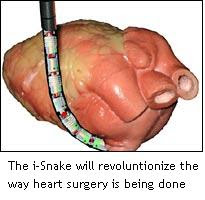
The CHR has faced ongoing financial pressures, largely because of Calgary's booming population and increasingly expensive medical technology.
The cash-strapped region has posted several deficits in recent years, including a $70-million shortfall last year and a $58-million deficit in 2004-05.
This year, shortages of nurses and other health workers have placed a new strain on the region's budget: overtime costs have climbed from $43.5 million last year to $63 million this year.
CHR is also picking up its share of the tab for a new contract the government signed with the province's registered nurses.
The deal, which makes Alberta's nurses the highest paid in Canada, came in higher than the CHR anticipated, leaving the region with a
$13-million unbudgeted expense.
In the past, when the CHR has run a deficit, the province has announced additional funding to help the health body remain in the black.
It is not yet clear if the government will offer the CHR additional funding to cover the deficit for the 2007-08 budget.
"Regions are required by legislation to balance their books," said Howard May, a spokesman for Alberta Health. "Those running deficits need to have a credible deficit elimination plan in place."
Laurie Blakeman, health critic for the Alberta Liberals, said the CHR could save money by hiring more nurses full time, rather than paying them time-and-a-half or double-time to work when they have a day off.
"It's penny wise and pound foolish, and we're paying the price for it," she said.
Davis said the region is already working to address the large number of part-time nurses at city hospitals and is discussing the issue with unions.
"In terms of part-time and full-time, we'll have to work with unions on something that works for everyone," said Davis.
The United Nurses of Alberta says this province has more part-time nursing jobs than any other Canadian jurisdiction.
Read the rest of the story here
The Ottawa Hospital will begin testing overnight patients for two virulent strains of bacteria beginning in January to help combat infections and deaths.